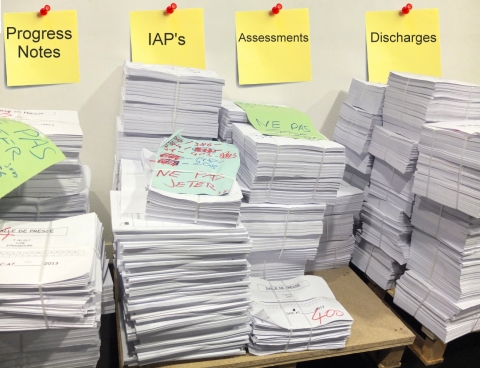
Go From This...
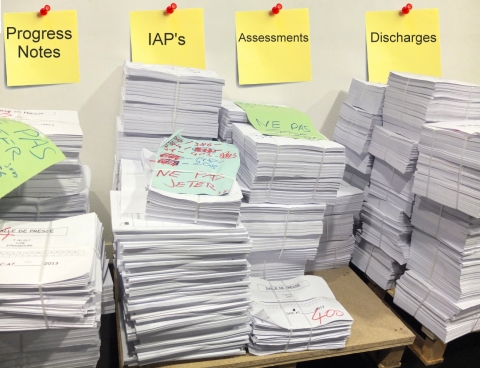
To This...


a complete Electronic Documentation System for
Outpatient Mental Health Professionals and Clinics

System Q is a software package; a complete electronic documentation system designed especially for outpatient mental health services and incorporates standardized clinical forms, quality standards, DSM-5 codes, descriptions and criteria and clinical guidelines and examples. The system automatically generates and routes documents and allows for efficient and improved management of client health records.
The software design has simplicity by eliminating unnecessary screen changes and complicated navigation. There is ease with the single screen design and interface is intuitive and concise. The system follows a prescribed document workflow for outpatient mental health services. Completeness is achieved with a comprehensive system that automatically generates and routes documents. All documents are accounted for. Administrators, directors and supervisors may easily track and monitor clinician performance and quality of service provided to clients. Professional and clinical competence is ensured with the use of standardized clinical forms, quality standards, DSM-5 criteria, and clinical guidelines and examples. The system assists and enhances clinical formulation, treatment planning, outcome measurement, quality assurance, and justification of ‘medical necessity’. The system prevents missing or lost revenue due to late or missing billing submission, inefficient scheduling, or insurance ineligibility. Regulatory compliance is achieved and best clinical and business practices are maintained.
Revenue is delayed when rendered services are submitted late or when other required documents are past due. Revenue is lost when rendered services are not submitted or submitted after the insurance provider’s billing period has expired. Most agencies are unable to accurately and efficiently track weekly rendered services and ensure accompanying documents are submitted to billing by their weekly cut-off. The ‘unknown factor’ is the percent of missing rendered services. On average, agency’s may be missing twenty to thirty percent of weekly revenue. Most directors and supervisors do not have the resources to manually cross reference clinician calendars with weekly submitted documents. It is not unreasonable that a clinic may lose one to two progress notes per full-time clinician per week. This translates to thousands of dollars of missing revenue each week. Many therapists procrastinate and even skip paperwork submission deadlines because documentation is time consuming, in addition to their full schedule and the emotionally demanding nature of providing therapy.
This system provides therapists with an easy means to keep organized and document quicker. It allows management and supervisors to monitor performance and quality of care. This system provides accountability!
Missing or incomplete documentation and failure to justify medical necessity and quality of care are critical and common issues during health record reviews and may result in high fines and/or a strict corrective action plans as enforced by insurance providers and federal and state regulations.
This system ensures documents are accounted for; information is complete; and data integrity is maintained. Quality assurance standards, DSM-5 criteria, and clinical guidelines and examples provided and incorporated in this system, ensure quality of care and justification of medical necessity.